- 2 Mins to read
- DarkLight
7. Remote monitoring
- 2 Mins to read
- DarkLight
7.1 eConsent/Remote Consent
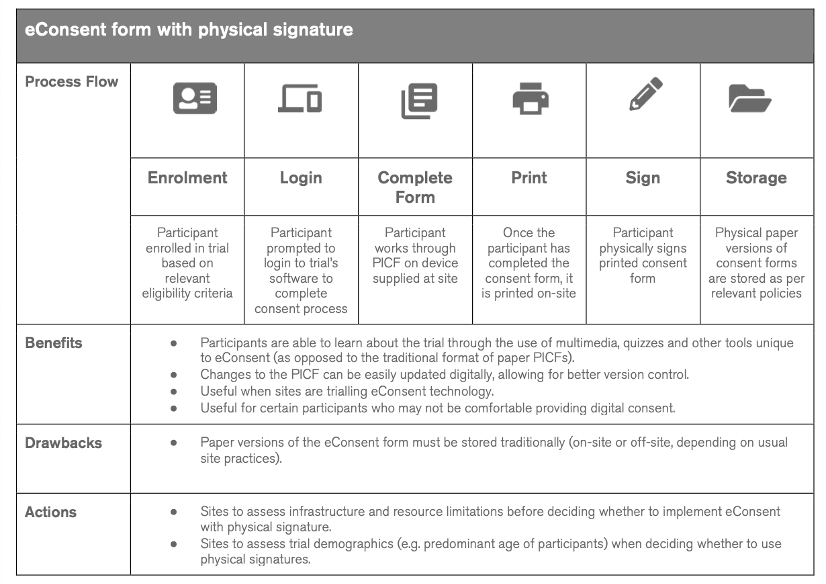
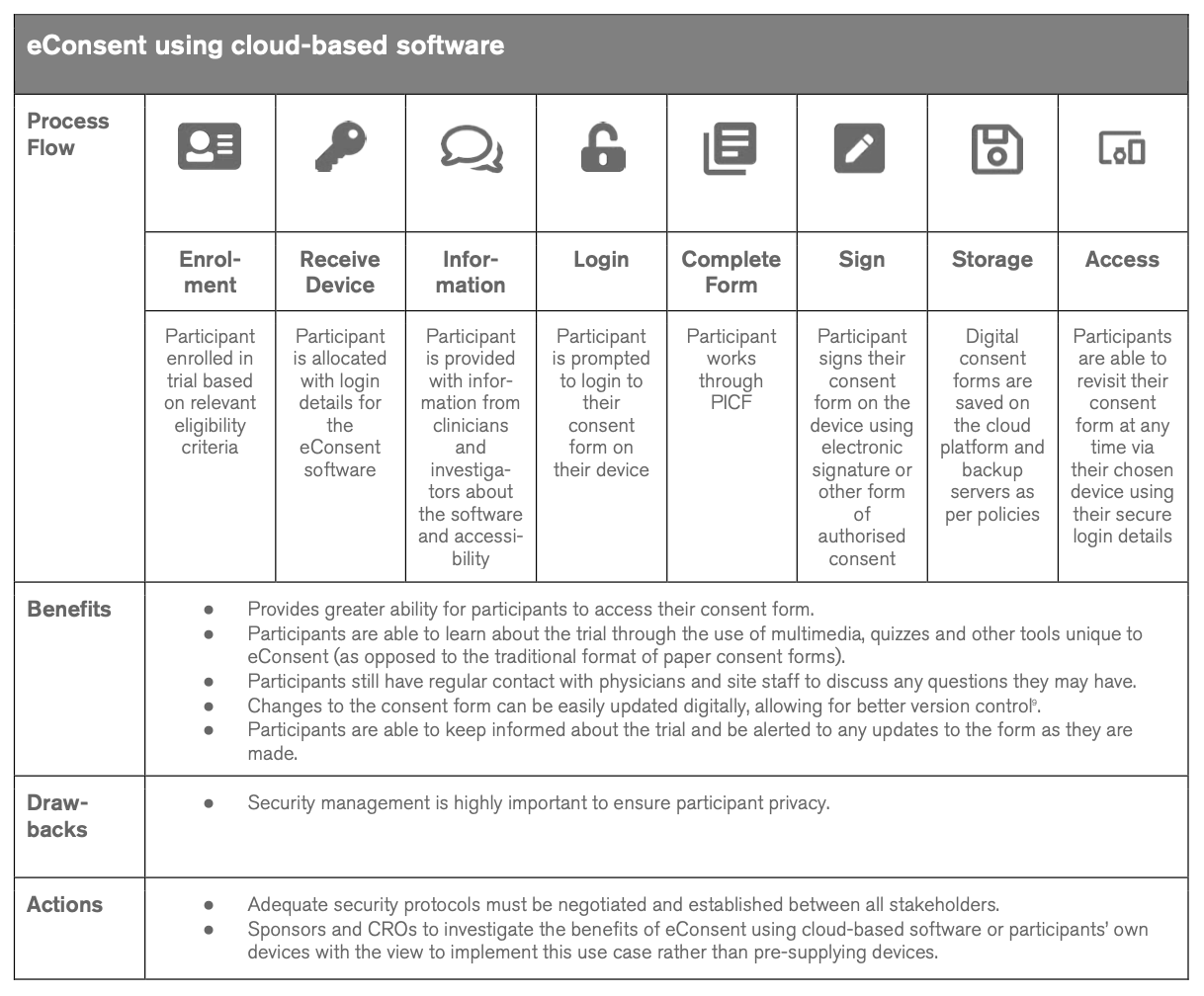
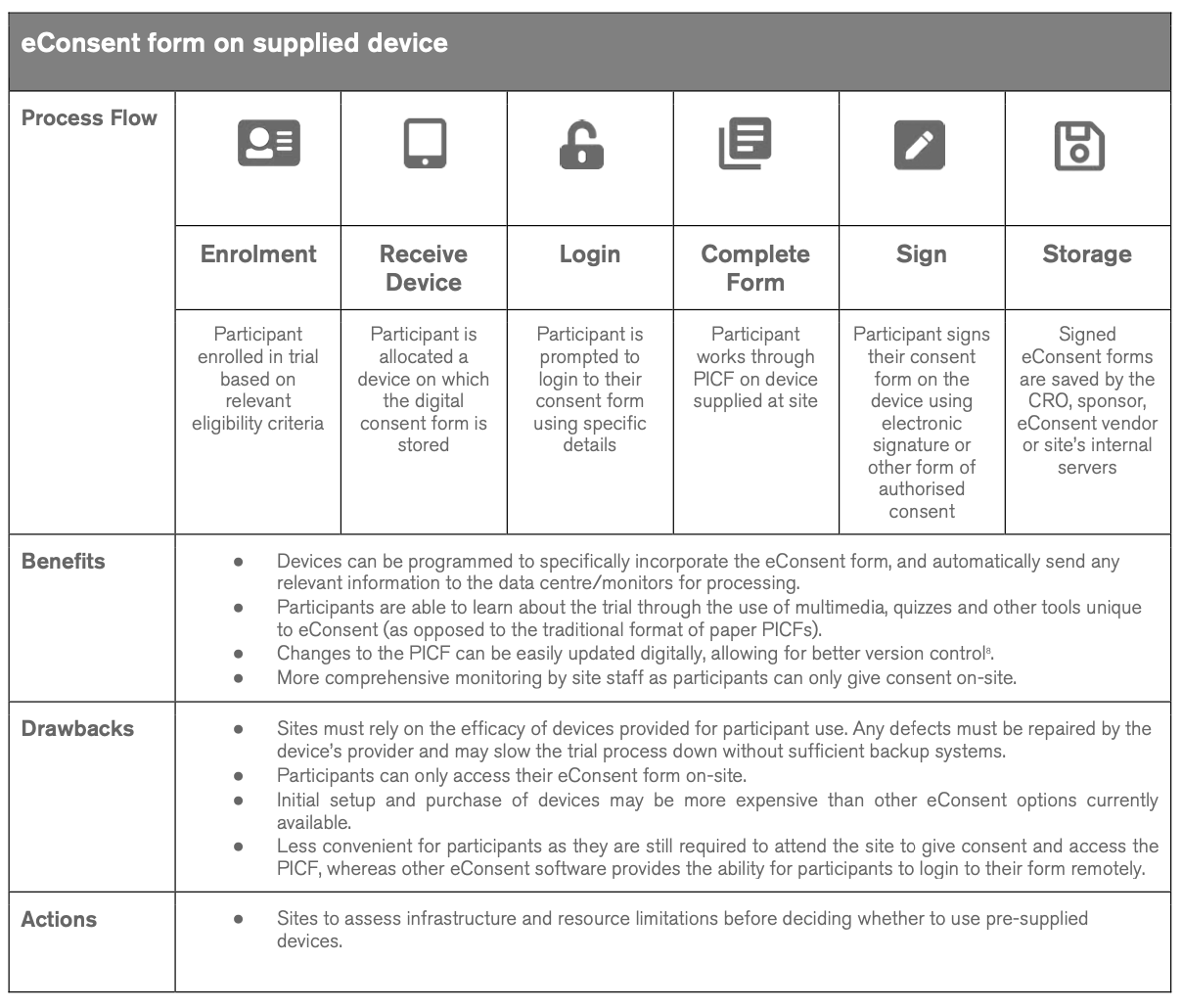
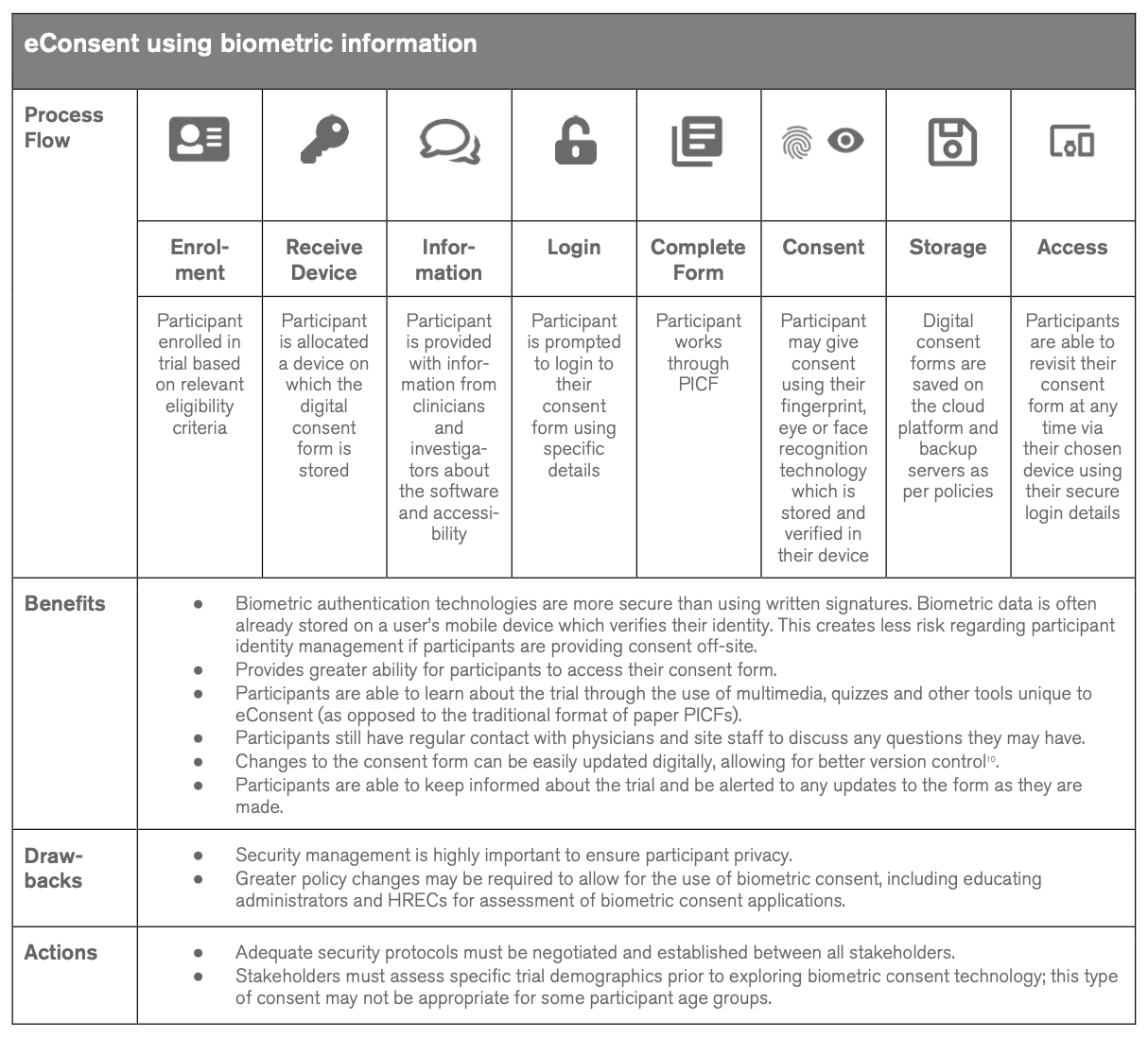
At present, eConsent use is not widespread in Australian clinical trials, although some trialing of eConsent software is occurring in an ad-hoc manner. Whilst a number of sponsors, CROs, and a handful of sites have investigated eConsent feasibility in Australia, approximately two-thirds of participants surveyed during this project had not been involved in a clinical trial with eConsent processes.
Australia itself has unique geographical barriers that may inhibit access to appropriate healthcare. With populations spread over vast distances and many people in regional or remote areas, it has been recognized through the teletrials initiatives recently funded by the State and the Federal Government that potential participants for clinical trials face significant barriers to accessing clinical trials. eConsent processes are currently being trialed for rural and remote participants. Adoption of eConsent technology in Australian trials may further enable greater reach and enhanced access to clinical trial information by participants located in geographically remote areas in ways that are impossible with paper-based approaches.
https://ctiq.com.au/wp-content/uploads/eConsent-in-Clinical-Trials-compressed.pdf
7.2 eSignature (including any requirement for a countersignature (e.g., PI, witness, etc.)
Yes, eSignature is permitted. See the National SOP for Clinical Trials. The PI or delegate must countersign and date that the consent process has occurred.
The local SOP does not make reference to ePro or DCTS specifically but allows the use of electronic systems for the collation and management of data.
7.3 Remote Assessment
Yes, remote assessment is permitted as defined in the National SOP for Clinical Trials which makes provisions for teletrials. This guideline was updated in July 2023 to reflect current practice.
7.4 Electronic Patient Reported Outcome (ePro)
Yes, ePro records are acceptable as defined in National SOP for Clinical Trials.
This guideline was updated in July 2023 to reflect current practice.
7.5 HHC – Home Nursing
Yes. There are no specific requirements but general standard procedures are described within the National SOP for Clinical Trials.
It is highly recommended to follow the process described under The National Rural and Remote Nursing Generalist Framework 2023–2027.
7.6 HHC – Home Lab Collection
Yes. There are no specific requirements but general standard procedures are described in https://www.health.gov.au/sites/default/files/2023-07/national-standard-operating-procedures-for-clinical-trials_0.pdf
7.7 Remote Monitoring
Yes. There are no specific requirements but standard procedures are described within the National SOP for Clinical Trials.
7.8 Telemedicine
Telemedicine is an accepted practice, especially in rural locations where access might be very limited. This has been used increasingly across Australia post the COVID-19 pandemic.
Australian Tele-Trial Model
The Australasian Tele-Trial Model was developed by the regional and rural group of COSA and uses telehealth to facilitate clinical trial activity. The purpose of the Model is to increase access to clinical trials for people with cancer living in rural and remote locations, although the benefits are not limited to this as it could also be utilized for patients with rare and less common cancers in metropolitan areas. COSA has led an MTPConnect funded project to pilot the Model over the last two years and the Model has now been implemented at sites in Queensland, NSW, and Victoria. There is significant interest and support for the Model from industry sponsors and investigator groups.
COSA has developed a range of resources to support the implementation of the Tele-Trial Model for sponsors and sites. The Tele-Trials resources webpage also provides links to other resources developed in Queensland, NSW, and Victoria to support the Tele-Trial Model.
7.9 Wearables
There is no specific guidance and this would need to be agreed upon by the HREC.
