- 9 Mins to read
- DarkLight
5. Investigator and Investigational Product
- 9 Mins to read
- DarkLight
5.1 Does local regulation require PI/CI to be approved/registered by any regulatory authority (e.g., RA/EC)?
The Principal Investigator must be a registered practicing physician with adequate experience and skills in running a clinical trial. There are no other specific requirements.
5.2 Does local regulation require any specific documents if PI/CI is based outside the country?
N/A.
5.3 Does local authority allow electronic ICF administration, including electronic signatures?
Yes.
5.4 Does local regulation require ICF to be administered as audio/visual and do these need to be recorded?
This is not mandatory. If consent is gained over the phone or by other means, the form needs to have a record of how this consent was gained.
5.5 Is there any specific information/requirement on data capture/management (e.g., privacy regulations, etc.)?
Data from clinical trials is governed by the Management of Data and Information in Research - A guide supporting the Australian Code for the Responsible Conduct of Research.
Key excerpt from the Australian Privacy Act 1988
95A Guidelines for Australian Privacy Principles about health information
Overview
1. This section allows the Commissioner to approve for the purposes of the Australian Privacy Principles guidelines that are issued by the CEO of the National Health and Medical Research Council or a prescribed authority.
Approving guidelines for use and disclosure
2. For the purposes of paragraph 16B(3)(c), the Commissioner may, by notice in the Gazette, approve guidelines that relate to the use and disclosure of health information for the purposes of research, or the compilation or analysis of statistics, relevant to public health or public safety.
Public interest test
3. The Commissioner may give an approval under subsection (2) only if satisfied that the public interest in the use and disclosure of health information for the purposes mentioned in that subsection in accordance with the guidelines substantially outweighs the public interest in maintaining the level of privacy protection afforded by the Australian Privacy Principles (disregarding subsection 16B(3)).
Approving guidelines for collection
4. For the purposes of subparagraph 16B(2)(d)(iii), the Commissioner may, by notice in the Gazette, approve guidelines that relate to the collection of health information for the purposes of:
- research, or the compilation or analysis of statistics, relevant to public health or public safety; or
- the management, funding or monitoring of a health service.
Public interest test
5. The Commissioner may give an approval under subsection (4) only if satisfied that the public interest in the collection of health information for the purposes mentioned in that subsection in accordance with the guidelines substantially outweighs the public interest in maintaining the level of privacy protection afforded by the Australian Privacy Principles (disregarding subsection 16B(2)).
Revocation of approval
6. The Commissioner may, by notice in the Gazette, revoke approval of guidelines under this section if he or she is no longer satisfied with the matter that he or she had to be satisfied with to approve the guidelines.
5.6 Does local regulation allow Home Healthcare Professional Visits (HHCP) in decentralized and/or hybrid studies? If yes, explain if there are any specific requirements to fulfill these obligations.
Yes. There are no specific requirements but standard procedures are described within the National Standard Operating Procedures for Clinical Trials, including teletrials.
It is highly recommended to follow the process described under The National Rural and Remote Nursing Generalist Framework 2023–2027.
5.7 Does local regulation allow Direct-to-Patient (DTP) study product delivery (such as home delivery) in clinical trials? Are there specific requirements to fulfill (e.g., acknowledgment of/signature for the product by the patient, etc.)?
Yes. There are no specific requirements but standard procedures are described within the National Standard Operating Procedures for Clinical Trials, including teletrials.
5.8 If a clinical study involves the study product as OTC and this is provided via pharmacy/Amazon, etc., are there any specific regulations for IP management that need to be followed?
No. The investigational product must be managed by a qualified pharmacist.
5.9 For a marketed study product/OTC, can a participant be compensated after confirmation of the purchased study product, or upfront prior to product acquisition? Does compensation in any way impact how the study is viewed (i.e., RWE vs. Interventional Study)?
No. In Australia, any product to be used as part of a trial (interventional or otherwise) needs to be provided in a controlled manner via the sponsor.
5.10 Is it permitted to pay participant stipends (i.e., is it permitted to pay the patients for their participation in the clinical trial)? If so, what is the average range?
The National Statement outlines that:
2.2.10 It is generally appropriate to reimburse the costs to participants of taking part in research, including costs such as travel, accommodation and parking. Sometimes participants may also be paid for time involved. However, payment that is disproportionate to the time involved, or any other inducement that is likely to encourage participants to take risks, is ethically unacceptable.
2.2.11 Decisions about payment or reimbursement in kind, whether to participants or their community, should take into account the customs and practices of the community in which the research is to be conducted.
Clinical trial participants are not required to be paid; however, they may be paid reasonable costs to cover their time and travel. Payments are on average $10 AUD per hour and no more than $360 AUD per day.
For further information on clinical trial payment please refer to the NHMRC guidance Payment of Participants in Research: information for researchers, HRECs, and other ethics review bodies 2019.
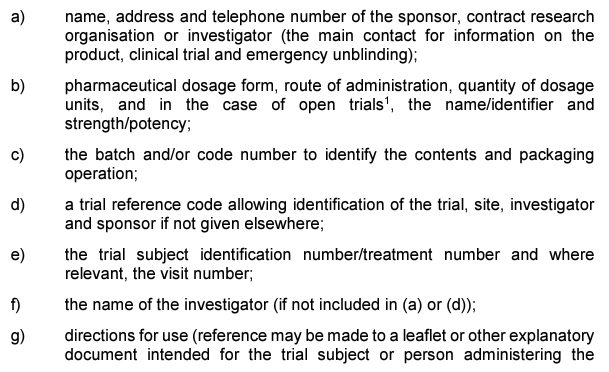
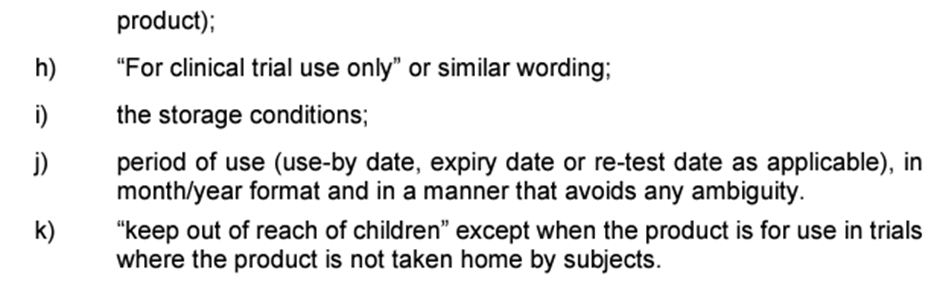
5.11 Specific labeling requirements for clinical study product
The labeling therapeutic goods orders TGO 69, TGO 91, and TGO 92 do not apply to investigational medicinal products. Instead, labeling requirements are specified in Annex 13 of the PIC/S Guide to Good Manufacturing Practice for Medicinal Products. This document outlines the information to be included on labels, unless its absence can be justified, for example, when using a centralized electronic randomization system.
Complete details on primary and secondary packaging and labeling requirements can be found in Annex 13 of the PIC/S Guide to Good Manufacturing Practice for Medicinal Products. The key elements required in the label are as follows:
Labeling and centralized electronic randomization systems
The labeling requirements of Annex 13 of the PIC/S Guide to Good Manufacturing Practice for Medicinal Products must generally be met, however, certain information may be omitted from the label where centralized electronic randomization systems (CERS) are used.
When CERS is used, investigational medicinal products are:
- distributed to participants to administer at home, the label should contain:
- sufficient information so that any person can readily identify the product if required (such as in an emergency), and
- the main contact for product information, clinical trial and emergency unblinding, and
- directions for use, and
- storage conditions and expiry, use-by or re-test date
- Administered by dedicated trial staff and no additional investigational medicinal product is retained by participants, it may be possible to:
- omit information (except the expiry date) from the labels in a readable format, provided that alternative means of accessing, verifying, and retaining relevant information are provided by the CERS.
The decision to omit certain information should be made according to risk management principles and information should be checked immediately before administering the investigational medicinal product.
Labeling biologicals
Investigational biologicals must comply with the labeling requirements set out in the Australian Code of Good Manufacturing Practice for Blood and Blood Components, Human Tissues, and Human Cellular Therapy Products. The exception is biologicals that comprise or contain live animal cells, tissues, or organs, which must comply with Annex 13 of the PIC/S Guide to Good Manufacturing Practice for Medicinal Products.
5.12 What documents need to be submitted (including relevant fee if any), and to whom, if a permit is needed for an investigational/study product being shipped from outside the country? Are there any specific requirements for biologics?
Import restrictions for therapeutic goods
A number of Restrictions may apply to the import of therapeutic goods for clinical trials. The key references are as below:
- Therapeutic goods legislation (see below)
- Customs (Prohibited Imports) Regulations 1956 and – a license and or permit to import or export may be required for substances controlled under this legislation
- Biosecurity Act 2015 – permission may be required prior to importing any material of biological origin (human, animal, plant or microbial)
- Environment Protection and Biodiversity Conservation Act 1999 – permission may be required prior to importing endangered species
- Gene Technology Act 2000 – permission may be required prior to importing genetically modified organisms
- State and territory requirements (contact the relevant state or territory department of health)
- Requirements of the legislation of the originator country
Importing therapeutic goods for use in clinical trials in Australia
The Therapeutic Goods Act 1989 prohibits the import into or supply in Australia of ‘unapproved’ therapeutic goods for use in humans unless they are included in the ARTG or otherwise the subject of an exemption, approval, or authority.
Item 1 of Schedule 5A to the Therapeutic Goods Regulations 1990 and item 2.1 of Schedule 4 to the Therapeutic Goods (Medical Devices) Regulations 2002 provides an exemption for therapeutic goods to be imported and held prior to supply in a clinical trial subject to conditions.
The imported therapeutic goods must be held under the direct control of the sponsor (importer) until the goods are the subject of a notification under the CTN scheme or approval under the CTA scheme. Until such time, the goods must be kept in a warehouse or a properly secured area under the control of the importer in accordance with the relevant exemption.
There is no requirement for the CTN or CTA process to have been completed prior to the importation of the clinical trial goods. However, approval through the CTA scheme or notification through the CTN scheme needs to have occurred prior to the supply of the goods to the trial sites.
Other conditions relevant to the exemption include keeping records relating to the source and supply of the goods. These records should be provided to us if requested.
Application for approval to import/export unapproved therapeutic goods for experimental purposes
You will need to apply for approval to import clinical trial goods for subsequent export or to export clinical trial goods manufactured in Australia.
Approvals are usually granted for multiple consignments for export to one or more countries for a period of twelve months. A new application is required to renew an approval after the twelve-month period. A new application is also required to obtain approval to export to additional countries. A report detailing the quantity of goods that have been exported to each clinical trial site must be submitted to the TGA every six months.
Additional requirements
Additional restrictions may be imposed on the import and export of unapproved therapeutic goods through the:
- Customs (Prohibited Imports) Regulations 1956- external site and Customs (Prohibited Exports) Regulations 1958- external site
- List of drug substances requiring permission to import and/or export for further guidance
- Quarantine Act 1908- external site
- Contact the Department of Agriculture- external site for information regarding quarantine clearance
5.13 What is the turn-around time to get an import permit?
TGA aims to process approvals within 15 working days from the date of receipt.
However, there will be times when high demand may result in slightly longer processing times.
5.14 Does local authority allow the destruction of clinical supplies at an off-site location (e.g. third-party vendor in or outside the country) after study completion? Are certificates of destruction required?
The Guideline for Good Clinical Practice outlines that trial sponsors need to maintain a system for the retrieval and disposition of investigational product(s) and for the documentation of this disposition.
There are provisions under the therapeutic goods legislation that allow the export of therapeutic goods for destruction. Under item 2 of Schedule 5 to the Therapeutic Goods Regulations 1990 and item 1.2 of Schedule 4 to the Therapeutic Goods (Medical Devices) Regulations 2002 ‘unapproved’ therapeutic goods may be exported from Australia if they:
- are not for commercial supply; and
- do not contain a substance the exportation of which is prohibited under the Customs Act 1901; and
- are not intended for use in clinical trials on humans.
Therefore, if the above conditions apply, then the goods may be exported for destruction without any requirement for export approval from TGA. There is no requirement for certificates of destruction.
