- 8 Mins to read
- DarkLight
10. Roadmap of the Submission Process of a Clinical Trial
- 8 Mins to read
- DarkLight
10.1 Clinical Trial with Investigational Medicinal Product
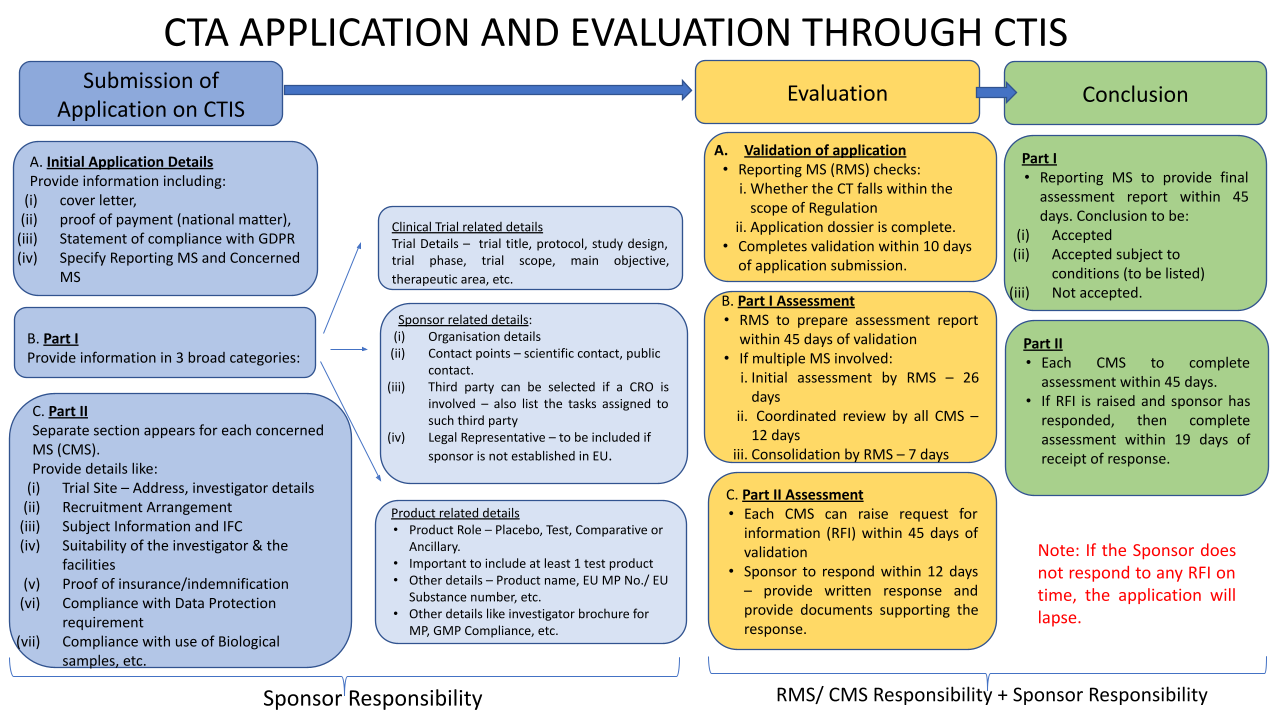
The submission process using CTIS is described in more detail below this flow chart/roadmap:
Training is to be prioritized for relevant staff in Belgium on the use of the Clinical Trial Information System (CTIS) - accessible via euclinicaltrials.eu.
The EU's new Clinical Trial Regulation (EU) 536/2014 came into force on 31st January 2022.
The aim of the EU CTR is to ensure a greater level of harmonization of the rules of conducting clinical trials throughout the EU. Subject to some transitional provisions, the EU CTR repeals the EU’s Clinical Trials Directive 2001/20/EC. The EU CTR features:
- A streamlined application procedure for all clinical trials conducted in Europe via a single EU portal and database. All applicants must be registered before submission of a clinical trial application.
- A single authorization procedure for all clinical trials, to allow a faster and more thorough assessment by all concerned EU countries.
- The extension of the silent agreement principle to the authorization process (After validation of the application (10 to 25 days), the assessment of Part I should last 45 days. The assessment for Part II, which runs in parallel, should also last 45 days. Then, each Member State Concerned has five days to give its decision on whether the trial may proceed, if a Member State does not provide its decision within the five-day timeframe, it will be understood that it has tacitly approved the assessment of Part I and that will conclude the Part I assessment report) giving more legal certainty to sponsors and researchers, in particular SMEs and academics.
- Strengthened transparency for clinical trial data the EU CTR aims to increase the availability of information on clinical trials through the EU clinical trial portal and database. Art 81(4) of the EUCTR states that the (information in the) EU database shall be publicly available unless confidentiality is justified, (e.g., in order to protect personal data or commercially confidential information). The CTIS serves as a key instrument to increase the transparency of clinical trials by offering searchable clinical trial information to patients, healthcare professionals, and the general public. Clinical trial results will be available as a technical summary and in lay language.
Implementation of the EU CTR is by way of a phased transition that will happen over a 3-year period, whereby, during that period, organizations who have clinical trials running, will progressively transfer ongoing clinical trials over to the new system in accordance with the rules of the EUCTR, at the latest by 31st January 2025. From 31st January 2023, all new applications for clinical trials must be registered using the new system established in the EU CTR.
The previous Clinical Trials Directive 2001/20/EC ('Clinical Trials Directive') is repealed with effect from 31st January 2022. The Clinical Trials Directive will, however, continue to apply until 31st January 2025 in respect of:
- Clinical trial applications submitted before 31st January 2022; and
- Clinical trial applications submitted before 31st January 2023, if the sponsor opted to submit in accordance with the Clinical Trials Directive (rather than via the EUCTR’s CTIS portal).
During the transitionary period EU Member States may continue to apply their national law, adopted to transpose Directive 2003/94/EC to those clinical trials conducted under the Clinical Trials Directive. In other words, EU Member States may continue to apply the current regulatory regime until 31st January 2025.
Submission of applications – Process
Under the new EU CTR, applications for trials with medicinal products in humans can be submitted through a new Clinical Trial Information System (CTIS) - accessible via euclinicaltrials.eu - along with amendments and other changes to ongoing clinical trials.
The CTIS includes workspaces for clinical trial sponsors and authorities as well as a public website. In order to access the CTIS Sponsor workspace, users need an active EMA account. Further, the users need to register their organization and trials via the Organization Management Service (OMS) from which CTIS retrieves its data. In addition, before completing the clinical trial application in CTIS, the sponsors should ensure that the details of the medicinal products used in the clinical trials are already registered in the eXtended EudraVigilance Medicinal Product Dictionary (xEVMPD). A placebo can be added manually in CTIS directly. Further, the active substance for the developed medicinal product must be available in EMA SMS (Substance Management Service).
Submission & Choice of Reporting Member State
The application is submitted via the CTIS portal by the Sponsor and will include details for all Concerned Member States (CMS) where the Sponsor intends to conduct the clinical trial.
The Sponsor will nominate a Reporting Member State who will act as the single point of contact with regard to the authorization process.
In terms of choosing the Reporting Member State, if the proposed Clinical Trial is deemed to be a low-intervention clinical trial Art.2.2 (3) EU CTR (e.g., the medicinal product has marketing authorization in one of the CMS, or it is an investigational medicinal product which is to be used in the Clinical Trial in accordance with published scientific data in relation to its safety and efficacy in one of the CMS) then the Member State to which this criteria applies should be nominated as the Reporting Member State.
Apart from these criteria, the EU CTR is silent as to the choice of the Reporting Member State. However, the Reporting Member State nomination may not always be granted, and it is on Day 6 following submission that the Reporting Member State is confirmed.
More information can be found in the EMA CTIS Sponsor Quick Guide.
10.2 Pediatric Investigation Plan (PIP)
A pediatric investigation plan (PIP) is a development plan aimed at ensuring that the necessary data are obtained through studies in children, to support the authorization of a medicine for children. All applications for marketing authorization for new medicines have to include the results of studies as described in an agreed PIP unless the medicine is exempt because of a deferral or waiver.
This requirement also applies when a marketing authorization holder wants to add a new indication, pharmaceutical form, or route of administration for a medicine that is already authorized and covered by intellectual property rights.
Deferrals and Waivers
The Pediatric Committee (“PDCO”) may grant PIP deferrals for some medicines. These allow an applicant to delay the development of the medicine in children until, for instance, there is enough information to demonstrate its effectiveness and safety in adults. Even when studies are deferred, the PIP will include details of the pediatric studies and their timelines.
Reporting under Deferrals
A. Annual Report
Marketing authorization holders who have received a deferral on a PIP are obliged to submit annual reports to the EMA. These reports should provide an update on progress with pediatric studies in accordance with the decision of the EMA agreeing on the PIP and granting a deferral.
- New medicines
If an agreed PIP for a new medicine contains a deferral, the applicant needs to send the first annual report to the Agency in the month before the first anniversary of the date of marketing authorization. There is no need to submit annual reports before the marketing authorization is granted.
- Medicines already authorized
- if the PIP decision is agreed upon less than six months before the anniversary date of the first marketing authorization granted in the European Economic Area, the marketing authorization holder should send the annual report in the month before the next anniversary of the date of the marketing authorization;
- if the anniversary date occurs more than six months after the date of the PIP decision, the report should be sent in the month before the anniversary date.
Use the date of the decision on the initially agreed PIP to calculate the due date of the first annual report. Do not use the date of any subsequent modifications of the agreed PIP.
B. Subsequent Reports
Subsequent annual reports need to be submitted every year, within the sixty days preceding the anniversary of the marketing authorization date.
The PDCO may also grant waivers when the development of a medicine in children is not needed or is not appropriate, such as for diseases that only affect the adult population.
Post Assessment
After assessing an application for a PIP, deferral, waiver, or modification, the PDCO formulates an opinion, which is notified to the applicant. The applicant is then able to request a re-examination of the opinion if s/he wishes. Once the Committee has issued its final opinion, after re-examination if requested, the EMA adopts a decision.
The EMA makes all opinions and decisions on PIPs, deferrals, and waivers public, after deletion of information of a commercially confidential nature.
Scientific Advice
Applicants can request scientific advice from EMA in preparation for a PIP, which is free of charge for questions relating to the development of pediatric medicines. They can also follow up a PIP with scientific advice, for example on combined adult and pediatric development in light of the PIP requirements.
EMA discourages applicants from submitting scientific advice and a PIP application in parallel.
For further information, please see the PIP-related page by the EMA.
10.3 Clinical Study (Interventional or Observational)
The Belgian Law of 2017 applies only to ‘clinical trials’ within the meaning of EU CTR 536/2014. The previous Belgian law of 7 May 2004, relating to experiments on the human person (“Law of 2004”) still applies to experiments on human beings outside the scope of the EU CTR 536/2014.
In the Law of 2004, “experiment” is defined as “any test, study or research carried out on a human person, for the development of the knowledge specific to the exercise of the health care professions.”
The Law of 2004 contains provisions surrounding consent of participating subjects, with special provision for minors or adults unable to provide consent for participation in trials, authorization of an experiment, obligations on the end of the experiment, obligations to report adverse events and serious adverse events, manufacture, import, distribution, and labeling of experimental drugs.
